Understanding Human Chorionic Gonadotropin (hCG)
In this comprehensive article, we delve into the multifaceted world of Human Chorionic Gonadotropin (hCG). hCG is a crucial chemical produced by trophoblast tissue, commonly found in early embryos and later forming a part of the placenta. The significance of measuring hCG levels spans various aspects, including pregnancy assessment, identification of pathologic pregnancies, and its relevance in the aftermath of an abortion. Additionally, hCG plays a pivotal role in detecting and managing various cancers, such as choriocarcinoma and extra-uterine malignancies.
Etiology and Epidemiology
Production and Origins: hCG primarily originates from syncytiotrophoblastic cells in the placenta during pregnancy. It acts by stimulating the corpus luteum to produce progesterone, essential for maintaining the pregnancy. While smaller amounts are produced in the pituitary gland, liver, and colon, certain malignancies can also produce hCG or hCG-related hormones, contributing to high serum levels in such cases.
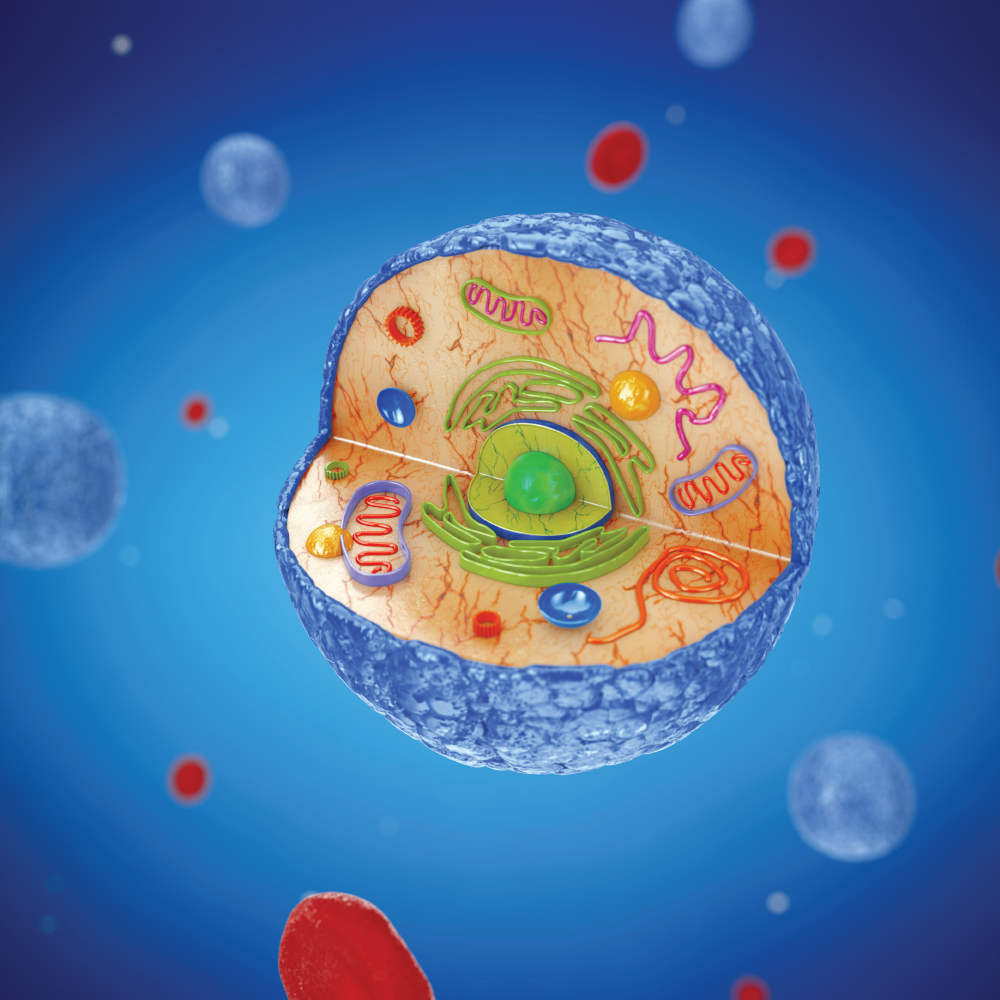
Glycoprotein Structure: hCG is a glycoprotein consisting of two subunits, alpha and beta. Multiple forms of hCG are present in the serum and urine during pregnancy, including intact hormoness and free subunits. Notably, the beta subunit undergoes degradation in the kidney, forming a core fragment that is measurable in urine hCG tests.
Specimen Requirements and Procedure
Urine Testing: Collecting urine for hCG testing requires attention to timing, as a diluted specimen can yield false-negative results. It’s important to avoid collection after the patient has consumed large amounts of fluids.

Blood Testing: Serum hCG tests involve obtaining a peripheral blood sample. These tests utilize immunometric assays that employ two antibodies binding to the hCG molecule, facilitating quantitative results.

Diagnostic Tests
Immunometric Assays: Serum hCG tests utilize immunometric assays employing two antibodies – a fixed antibody and a radiolabeled antibody. These antibodies bind to different sites on the hCG molecule, creating a sandwich effect that immobilizes the molecule for detection. Notably, there’s a wide range of commercially available assays, leading to variability in reported values.
Urine Assays: Urine tests are similar to serum tests but are generally less sensitive. Many over-the-counter urine pregnancy tests may not detect hyperglycosylated hCG, which is predominant in early pregnancy.
Testing Procedures
Urine Testing: Urine is placed in a designated receptacle, typically a commercially available test. A positive result is indicated by the appearance of an indicator (such as a colored line), along with a control line. A negative result shows only the control line.
Serum Testing: Serum hCG testing is performed in a laboratory setting using peripheral blood samples. Special precautions, such as dilution in cases of suspected gestational trophoblastic disease, may be necessary.
Interfering Factors
It’s crucial to be aware of potential reasons for false hCG test results, which can have significant clinical implications.
Serum False Positives: These may be caused by ectopic hCG production, heterophile antibodies, rheumatoid factors, IgA deficiency, or even exogenous hCG preparations for weight loss or assisted reproduction.
Serum False Negatives: Early measurement after conception and the “Hook effect” can lead to false negatives. Dilution prior to testing is advisable in cases of suspected gestational trophoblastic disease.
Urine False Positives: Factors such as blood or protein in the urine, human error in result interpretation, ectopic hCG production, exogenous hCG, or certain drugs can result in false-positive urine tests.
Urine False Negatives: Early measurement after conception, dilute urine specimens, and the “Hook effect” can lead to false-negative urine test results.
Results, Reporting, and Critical Findings
HCG levels are typically reported in milli-international units of hCG per milliliter of blood (mIU/mL). Urine hCG testing provides qualitative results (positive or negative), with a typical detection threshold of 20 to 50 mIU/mL. Serum assays offer greater sensitivity, measuring beta-hCG levels as low as 1 to 2 mIU/mL.
Clinical Significance
Pregnancy
In pregnancy, hCG is a vital hormone. Its clinical utility encompasses early pregnancy detection, serial measurement during pregnancy, and addressing pregnancy-related complications. hCG levels exhibit significant variation among women with normal pregnancies. Typically, they rise exponentially in the first trimester, doubling approximately every 24 hours during the first 8 weeks.

Patients with plateaued hCG levels or failure to double before 8 weeks often have nonviable pregnancies, which may be intra-uterine or extra-uterine (ectopic). Ectopic pregnancies typically show low rate-of-rise in hCG levels. Serial measurement and ultrasound evaluation are recommended to enhance diagnostic accuracy.
Return to Zero
HCG levels typically return to zero within 7 to 60 days following delivery or pregnancy termination. Trending the fall of hCG levels is essential, especially in the case of molar pregnancies or post-pregnancy/ectopic pregnancy terminations, to confirm the effectiveness of therapy.
Clinical Implications
The variety of antibodies used in commercial assays can lead to significant variability in immunoassay results. This is particularly relevant when comparing results from different laboratories or facilities, especially when examining low values post-pregnancy termination or trophoblastic disease.

Gestational Trophoblastic Disease
HCG detection is valuable in evaluating various trophoblastic diseases, including complete and partial hydatidiform mole, postmolar tumor, gestational choriocarcinoma, testicular choriocarcinoma, and placental site trophoblastic disease. Different levels of hCG are reported on commercial assays for these conditions, aiding diagnosis, treatment assessment, and monitoring for recurrence or disease persistence.
Non-Pregnant Patients
In nonpregnant women, serum hCG levels can increase with age. A cutoff of 14 mIU/mL has been suggested for interpreting results in women over the age of 55. Persistently positive hCG testing in nonpregnant patients should prompt evaluation for conditions such as testicular cancer, ovarian cancer, bladder cancer, or other malignancies.
Enhancing Healthcare Team Outcomes
Understanding the utility and variability of different hCG assays is critical for healthcare providers across disciplines. False-positive and false-negative test results can have significant impacts on patient care. Collaboration, shared decision-making, and effective communication within the healthcare team are essential to optimize patient outcomes.
In conclusion, Human Chorionic Gonadotropin is a multifaceted hormone with diverse clinical applications, ranging from pregnancy assessment to cancer detection and monitoring. Awareness of potential interfering factors and assay variability is crucial for accurate diagnosis and patient care.